Which Of The Following Can Change The Frequency Of Resistant Cells In A Population Of Bacteria?
Measures of Illness Frequency
Introduction
For centuries, knowledge about the crusade of disease and how to treat or prevent information technology was limited by the fact that information technology was based almost entirely on anecdotal evidence. Pregnant advances occurred when the strategy for studying illness shifted to looking at groups of people and using a numeric arroyo to make critical comparisons.
Learning Objectives
Subsequently successfully completing this section, the student will be able to:
- Ascertain what is meant by the term 'population' in both descriptive epidemiology and analytic epidemiology.
- Explicate the difference between fixed versus dynamic populations.
- Explain the differences among the parameters: ratio, proportion, & rate.
- Define and calculate prevalence (and be able to distinguish betwixt point prevalence and period prevalence). Be able to explain the use of prevalence in public health.
- Define and distinguish between cumulative incidence and incidence rate, and describe their strengths and limitations.
- Explain the human relationship between incidence rate and cumulative incidence, and be able to compute an guess of CI from IR.
- Summate cumulative incidence and incidence rate from raw information and convert it into a course that enables you to compare the incidence in two or more groups.
- Explain what is meant by the term "at chance."
- Explain what is meant by "person-years" of ascertainment and exist able to calculate person-years of observation from raw data.
- Explain the interrelationship amidst prevalence, incidence, and average elapsing of affliction (i.e. P = IR x D). Be able to summate the average duration of illness, given the prevalence and incidence rate.
- Explain and calculate:
crude rates
category-specific rates (eastward.thousand. gender or race)
age-specific rates
- Be able to define and calculate the following special types of frequency measurements:
morbidity charge per unit
mortality charge per unit
example-fatality rate
set on charge per unit
live birth rate
infant mortality rate
autopsy charge per unit

Variables
Video Discussion of What Variables Are (2:43)
Link to transcript of the video
'Population'
A population is simply a group of people with some common characteristic, such as age, race, gender, or place of residence. A "target population" is a population for which y'all would like to make some conclusions. Examples:
- residents of Mumbai
- members of Blue Cross/Blue Shield (a U.Southward. wellness insurance organization)
- postmenopausal women in Massachusetts
- coal miners in Pennsylvania
- male person physicians in the Us
- members of the BUSPH intramural softball team
Stock-still versus Dynamic Populations
- Fixed population: In a stock-still population membership is relatively permanent and possibly defined past some event. Once a person experiences the defining event they remain part of that population as long every bit they are alive. Examples of relatively stock-still populations might include:
survivors of the diminutive blasts in Japan,
veterans of the Vietnam war or the Gulf Wars
members of the U.Due south. war machine who sustained a head wound while stationed in Iraq
residents of New Orleans who lost their homes during hurricane Katrina.
all babies born in Tanzania in 2012
Enrollment in an epidemiological study can also be the defining event for a person to enter a fixed population:
Persons who completed and returned a questionnaire in response to an invitation to bring together the Black Women's Wellness Study, and who were found to exist eligible by study staff
Residents of Boston public housing who met eligibility criteria, completed informed consent and a baseline survey, and had ane meeting with a community health worker to discuss smoking abeyance
- Dynamic population: In a dynamic population, membership is divers by current status, and then membership is non necessarily permanent. A person is a member of the population as long every bit they come across the definition of the population, and they end to exist a members of the population when they no longer encounter the definition. Annotation that a person tin be a member, leave, and and so become a member again. Examples of a dynamic population include:
residents of whatsoever boondocks or, land, or state
members of a health insurance programme
women who have given birth inside the past 12 months

It can be a fleck challenging at times to distinguish between fixed and dynamic populations, because the same clarification (e.g., resident of Boston) tin be interpreted as an effect or a current country. At that place are two helpful solutions to help clear upwardly this confusion:
- Ask for a clearer description. For example, compare "ever lived in Boston for at least one 24-hour interval" and "currently lives in Boston ". The first describes a stock-still population, the second a dynamic one.
- Think about why you are interested in the population. If we are interested in a question that is but relevant while the person lives in Boston, such as risk of accidents while riding a bicycle, then the population is dynamic, because once a person moves out of Boston there is no reason to follow them. On the other hand, if we are interested in a question that remains relevant even after a person leaves the city (east.thousand., does exposure to pollution atomic number 82 to later development of disease), and so you would want a fixed population.
Ratios, Proportions, and Rates
Ratio: A ratio is just a number that is obtained by dividing ane number by some other. A ratio doesn't necessarily imply any particular relationship between the numerator and the denominator. For example, if at that place were 100 women in this course and 20 men, the ratio of women to men would exist 100/20 or 5 women for each human being. This is only a unproblematic ratio that indicates how many times larger one quantity is compared to the other.
Proportion: A type of ratio that relates a part to a whole; oftentimes expressed as a percentage (%). For example, if at that place are 120 women in a grade of 130 students, and then the proportion of women is 120/130 = 92%.
Rate: A type of ratio in which the denominator also takes into account another dimension, usually time. For instance, speed is measured in miles/hr; it tin can be calculated by dividing the number of miles traveled by the number of hours that information technology took. H2o flow might be quantified in gallons/infinitesimal; ane might measure the number of gallons released during a menstruum of time and separate by the number of minutes it took in order to calculate the average rate. An example of a charge per unit that doesn't involve time is motor vehicle deaths, which are often reported equally deaths/vehicle-miles. This is 1 way in which the relative safe of dissimilar types of transportation (automobiles, buses, trains, airplanes) can be compared.
While the term "rate" is used very broadly among the general population (nascency malformation rate, autopsy rate, smoking rate, smoking rate, tax rate), in reality all these measures are proportions. For instance, the smoking "rate" amongst adults is actually the number of adults in a population who smoke divided by the total number of adults in the population—in other words, a proportion because the numerator is a subset of the whole. One fashion to tell a proportion from a true rate is that a charge per unit tin never exist expressed as a percentage, while a proportion should always be able to be expressed every bit a percentage.
Counts of Diseased People
Counting the people with disease is an of import basic measure out of disease frequency that is essential to detecting trends or the sudden occurrence of a problem, such as an epidemic. Simple counts of the number of diseased people are also important to public health planners and policy makers for assessing the need for resource in a population.
Table - New AIDS Cases past Year
| Yr | Total AIDS Cases in Metropolis A |
|---|---|
| 2001 | 0 |
| 2002 | one |
| 2003 | v |
| 2004 | 22 |
| 2005 | 75 |
The count of AIDS cases shown here for City A would probable stimulate discussion among public officials & health providers, but count data alone don't allow us to fully sympathize the problem. We don't know if all of the cases were long time residents who developed AIDS while living in City A. Some may have moved into town after they developed AIDS. We also don't know whether whatever of the cases moved away or died.
A second limitation of just counting the number of existing cases is that it doesn't allow us to make fair comparisons of the frequency of HIV in different cities, since they don't take into account the total number of residents.
When measuring disease frequency, proportions and rates are very helpful when comparing groups, because they relate the number of people with disease to the size of the population in which they occur. Prevalence and incidence are the two fundamental measures of disease frequency.
Suppose, for case, that City A had 75 HIV+ residents, while City B had 35. This would advise a larger problem in City A.
Table - Existing Cases of HIV+ in Cities A and B
| Existing Cases | |
|---|---|
| City A | 75 |
| City B | 35 |
However, suppose City A was substantially larger, with thirty,000 residents, compared to only vii,000 in Metropolis B. To be fair, i would need to take this into account past dividing the number of cases in each city by the respective population size.
Tabular array - HIV+ Cases, Population Size, and Prevalence in Cities A and B
| Existing Cases | Population Size | Prevalence | |
|---|---|---|---|
| Urban center A | 75 | 30,000 | 0.0025 |
| City B | 35 | 7,000 | 0.0050 |
In essence, the resulting decimal fractions indicate the frequency of HIV per person in each city, and we can at present see that Urban center B really has a higher prevalence of HIV+ residents than Metropolis A, in fact twice as high (0.005 vs. 0.0025). However, the frequency of HIV per private is not a very intuitive or useful concept. However, if we multiply each of the results ten x,000, we have the frequency per 10,000 population. Obviously, neither city has exactly 10,000 residents, but by converting the decimal fractions to this standard population size, we can now have a more understandable description of the prevalence of HIV+ residents in each city.
| Existing Cases | Population Size | Prevalence (as a decimal fraction) | Prevaence (per ten,000 population) | |
|---|---|---|---|---|
| City A | 75 | 30,000 | 0.0025 | 25 per 10,000 |
| Metropolis B | 35 | 7,000 | 0.0050 | fifty per 10,000 |




Prevalence
The measure of disease frequency nosotros have calculated is the prevalence, that is, the proportion of the population that has disease at a item time. Prevalence indicates the probability that a member of the population has a given condition at a point in fourth dimension. Information technology is, therefore, a way of assessing the overall burden of illness in the population, so it is a useful measure for administrators when assessing the need for services or treatment facilities.
Epidemiologists sometimes make a distinction between point prevalence , the proportion of the population at a 'betoken' in fourth dimension. And so it includes all previous cases who are still have the condition and are still members of the population. A good fashion to remember about signal prevalence is to imagine that yous took a snapshot of the poplation and adamant the proportion of people who had the condition of interest at the time the snapshot was taken.
Instance: The percentage of a class reporting symptoms of seasonal allergies during the offset week in May 2016.
Period prevalence is like to indicate prevalence, except that the "point in time" is broader. For example, suppose that 2,477 residents of Framingham, MA were examined the institute the proportion of the population that had cataracts. It may have taken 2-iii years to conduct all of the eye exams, and when they were washed the prevalence over this observation period would include people who had acquired cataracts previously if they still lived in that populations, and information technology would also include newl cases, i.e., those who had developed cataracts during the ii-iii twelvemonth period when the middle exams were conducted. So, it can just exist thought of as a broad "signal in time".
Example: During 1980 the Framingham Het Study examined two,477 subjects for cataracts and institute that 310 had them. Then, the prevalence was 310/2,477 = 0.125.
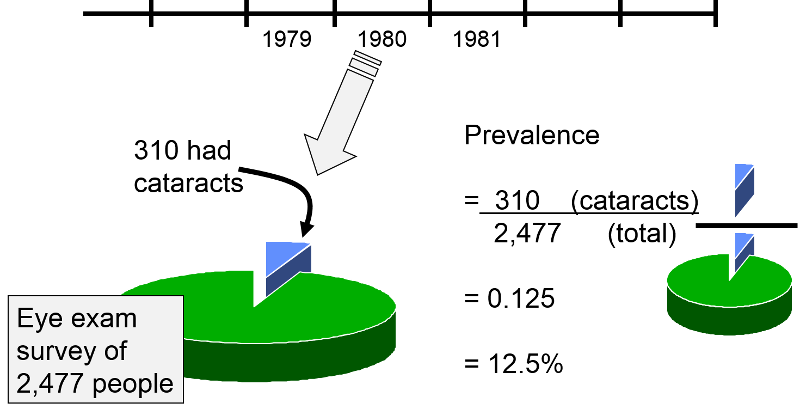
This can conveniently exist expressed every bit 12.5 per 100 or 12.five% (per cent means 'per hundred'). Since the examination of these subjects took place over a year, it might be referred to equally a menstruation prevalence, and the numerator conceivably could include people who had start developed cataracts prior to 1980 and people who developed cataracts during 1980 just earlier their examination was done. Note that all people counted in the numerator are also included in the denominator, i.e., the numerator is a subset of the denominator.
Frequently, this stardom between point prevalence and menses prevalence is blurry, because information technology is rare to be able to assess the proportion of a population that has a disease condition at exactly the same indicate in time. We could consider our class to be a population, and I could enquire the students to heighten their manus if they had an upper respiratory tract infection today. I could fifty-fifty take a photo and use this to visualize the prevalence of respiratory infections at this betoken in time. So, in this case this snapshot of affliction frequency in the class would truly correspond prevalence at a indicate in time. In almost cases, notwithstanding, information technology takes much longer than an instant to assess the proportion of a population that is diseased. In other words, we take to exist flexible in our definition of a "point" in time, and we take to allow for wide points. Regardless, of this stardom between point prevalence and period prevalence, the more than important concept is that prevalence is a measure of the proportion of the population that has a given disease, status, or characteristic at a given time. We will not try to distinguish point and menstruation prevalence in EP713.

Notes on Prevalence
Note that we can also use prevalence to assess the frequency of behaviors or characteristics that might be risk factors for disease. Smoking isn't a disease per se; it is a run a risk factor. All the same, information technology is relevant to appraise the prevalence of this beliefs.
Also, annotation that the "bespeak in fourth dimension" can be an event rather than a distinct agenda time. For case, many elderly men are found to have prostate cancer on autopsy, even though they were unaware of information technology and died for other reasons. It is appropriate to think of the frequency of prostate cancer at the time of autopsy as prevalence, even though men are having autopsies performed at many different points in calendar fourth dimension. Similarly, military recruits undergo a concrete examination during consecration, and the exams are performed at many unlike times. Nevertheless, the proportion of inductees establish to exist colorblind during their physical exam would be the prevalence of colorblindness in immature men.
Note that prevalence is a proportion and non a charge per unit, although the latter term is often used. Then, the terms "prevalence charge per unit" and "autopsy rate" are technically wrong (although unremarkably used).
Question: When calculating betoken prevalence, what should y'all do with people who were in the population, but they died or moved out of the population?
Reply

Incidence: Take chances, Cumulative Incidence (Incidence Proportion), and Incidence Rate
In dissimilarity to prevalence, incidence is a measure of the occurrence of new cases of illness (or some other issue) during a span of time . At that place are ii related measures that are used in this regard: incidence proportion (cumulative incidence) and incidence rate. A useful style to recollect near cumulative incidence (incidence proportion) is that information technology is the probability of developing illness over a stated period of fourth dimension ; as such, it is an guess of risk . Ken Rothman uses the example of a newspaper article that states that women who are 60 years of age have a two% risk of dying from cardiovascular illness. As written this argument is incommunicable to interpret, because it doesn't specify a fourth dimension menses. In club to interpret adventure it is necessary to know the length of time that applies. A two% run a risk has a very different meaning if it is over the next 12 months vs. the next 10 years. Therefore, the incidence proportion (cumulative incidence) must specify a fourth dimension catamenia. For example, the incidence proportion of neonatal mortality is the number of deaths divided by the number of births over the first 30 days after nativity.
The concept of risk is adequately intuitive - if a grouping of disease-gratis people were followed for a catamenia of time, one could determine the proportion of people who developed the illness at some signal during the observation period in gild to arrive at an estimate of the probability of developing that disease, i.e. the run a risk. However appealing this is for its simplicity, there are some drawbacks to this approach to assessing the occurrence of health outcomes, because an accurate assessment of probability relies on observing all subjects for the entire ascertainment period. This is peculiarly a problem when assessing long term risk.
- Commencement, in that location are competing risks that might result in the death of some subjects before the observation menstruation ends, making it impossible to know whether they would have developed the outcome of involvement if they had not died early because of some other take chances. For example, studying the incidence proportion of long term wellness conditions amidst soldiers in a disharmonize zone is complicated by the elevated take chances of dying in combat before the outcome tin be observed.
- A second problem is that, even if subjects don't die for another reason, it is difficult to follow people for long periods of time, and subjects can go lost to follow-upwardly , which too means that their outcome status is unknown.
- A tertiary problem is that the incidence proportion doesn't distinguish when a disease occurs every bit long as it is within the follow-up period. For example, if a population is followed for twenty years, it would brand a divergence to the person and to the epidemiologist if the cancer occurred after two years or after 20 years, but both of these outcomes would count the same with the incidence proportion.
For this reason, the incidence proportion is generally used in situations where the follow-up fourth dimension is relatively short and at that place is relatively fiddling loss to follow-up. Otherwise, epidemiologists generally use the incidence rate.
Ideally, if we are to approximate incidence (incidence proportion or incidence rate), nosotros would want to measure out this in a sample of people who are truly at risk of developing the issue of interest. So, in measuring incidence we would similar to exclude anyone who was not at risk of developing disease, because they already had the disease or considering they couldn't develop information technology. For example, if one wanted to judge the run a risk of developing uterine cancer in postmenopausal women, we ideally would like to exclude women who had previously undergone hysterectomy (removal of the uterus), since they are no longer at risk of developing this particular type of cancer.
Diabetes in a Nursing Home
 Suppose nosotros were interested in the trouble of diabetes in a nursing domicile with 800 residents. We would begin by doing blood tests on all residents to determine which were diabetic. If fifty of the residents were diabetic initially, then the prevalence of diabetes at this point in time would exist fifty/800 = 0.0625. The standard mode of expressing this would be to say that the prevalence was 62.5 per g residents or six.25 per 100 residents, or 0.0625%
Suppose nosotros were interested in the trouble of diabetes in a nursing domicile with 800 residents. We would begin by doing blood tests on all residents to determine which were diabetic. If fifty of the residents were diabetic initially, then the prevalence of diabetes at this point in time would exist fifty/800 = 0.0625. The standard mode of expressing this would be to say that the prevalence was 62.5 per g residents or six.25 per 100 residents, or 0.0625%
If nosotros want to judge the incidence of diabetes in this population over the next 12 months, we demand to exclude the 50 people who are already diabetic and focus on the 750 residents who are disease-free initially. We would and so need to do boosted blood tests to determine how many new cases developed during the span of time. Considering some of the residents might die or be transferred to other facilities during the year, nosotros ideally would like to take claret tests oftentimes, but for fiscal and logistical reasons, nosotros might simply carry a second series of blood tests after 1 year. If 25 were found to exist diabetic at the end of a yr, then the incidence would be 25/750 = 0.0333 or nigh three.three per hundred (3.3%) over a twelvemonth. Note that we are describing the time span, i.e. the flow of observation, when nosotros study the incidence.
When incidence is determined in this way, that is, past evaluating the presence of disease at the beginning so dividing the number of known new cases by the number of people "at hazard" at the beginning, it is referred to as a cumulative incidence and can also be idea of as the incidence proportion . While people commonly refer to this as a 'rate,' this is really a proportion. Information technology is the proportion of the "at take chances" group that adult disease over a stated block of time.
The cumulative incidence of AIDS in MA during 2004:
Cumulative incidence is easy to measure out and is unremarkably used in a wide variety of circumstances. For example, if we wanted to determine the incidence of AIDS in Massachusetts during agenda year 2004, it isn't viable for us to check every citizen at the beginning and end of the year. Census information gives united states a crude idea of how many people lived in Massachusetts during 2004, and AIDS is a reportable affliction, so we could get to the MA Section of Public Health and obtain an estimate of the number of people with AIDS at the starting time of the twelvemonth, and nosotros could subtract this number from the population size to get a denominator that represents the number of people "at risk" of developing AIDS. Then, we could go back to DPH at the finish of the calendar year and enquire how many new people had been reported with AIDS. This is our numerator. So, the cumulative incidence would be:
(# new AIDS cases reported during the year) / (population of MA at risk),
i.e. minus existing cases at the kickoff of the year)
In reality, there were 523 new AIDS cases reported in MA in 2004, and the population was about five.7 million. And so, the cumulative incidence was about 9.2 per 100,000 people during 2004. Note that the denominator is just an estimate based on the last census. In reality, people were being added to and subtracted from the population continually as a upshot of births, deaths, moving into the metropolis, and moving out. Nosotros also didn't have into account exactly when they developed AIDS, although we probably don't care whether they developed it earlier or later within a one year period. Withal, this cumulative incidence is a useful number, and it is relatively piece of cake to get the information we need to summate it.
It is important to specify the fourth dimension period when reporting cumulative incidence. In the autumn semester of 2003 in that location were 130 students in EP713 at the kickoff of the semester, and 55 of them reported developing a common cold or other respiratory infection during the semester. So, the cumulative incidence = 55/130 = 0.42307 or 42.iii% over the course of the semester. The time catamenia of observation is expressed in words.
Incidence Rate
Remember that a rate most e'er contains a dimension of fourth dimension. Therefore, the incidence rate is a mensurate of the number of new cases ("incidence") per unit of measurement of time ("rate"). Compare this to the cumulative incidence (incidence proportion), which measures the number of new cases per person in the population over a defined catamenia of fourth dimension. Considering studies of incidence in epidemiology are conducted among groups of people every bit they motility through fourth dimension, the denominator is really a combination of the number of people and the amount of time. This is expressed as person-time. The time units can be expressed in days, months, or years, but should exist tied to the length of the written report and assist interpretation of the results. The most frequently encountered expression is "person-years". The characteristics of cumulative incidence and incidence rate are illustrated in the examples beneath.
Note: While we generally refer to cumulative incidence (incidence proportion) and incidence charge per unit as measures of affliction frequency, they can exist applied to any sort of occurrence. For example, treatments to cure or relieve illness conditions are also measured using the incidence proportion or rate, as we will run into in the example below. The key thing to keep in mind is that either measure of incidence (different prevalence) measures a transition from one country to some other: well to sick, sick to well, alive to dead, unborn to born, etc.
A comparison of pain relief with ii analgesics:
Suppose you were asked to analyze the information from a small preliminary clinical trial with 20 subjects. All subjects had a comparable degree of knee hurting from osteoarthritis, and they were being compared with respect to pain relief afterward receiving a standard hurting medication (Drug B) or a new pain medication (Drug A). The 20 patients were randomly assigned to one drug or the other, and at that place were ten subjects in each group. After receiving the medication, the investigators checked on the subjects at hourly intervals to see if the subjects had had relief of hurting. For each subject field, the fourth dimension at which pain relief occurred was recorded. Results are illustrated in the graph below. Link to a text description of the results
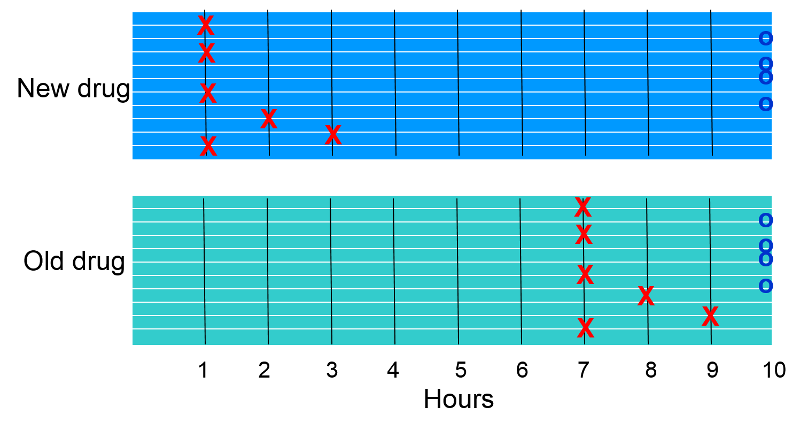
The "X"s betoken when subjects reported pain relief. The "O"southward at the stop bespeak subjects who did not report relief of pain.
- Which group appears to have had a greater incidence rate of pain relief?
- How did the cumulative incidence of pain relief compare (the proportion of subjects experiencing pain relief)?
Cumulative Incidence
Six of ten subjects in each group experienced relief of hurting, so the cumulative incidence of pain relief was 6/10 = 60% in each grouping. Whenever cumulative incidence is adamant, one determines the proportion of subjects who experienced the outcome of interest during a block of time, without taking into business relationship when subjects developed the issue. Visually, even so, it is articulate that if we consider when subjects experienced relief, the rate was greater in the subjects receiving the new drug.
Incidence Rate
In this hypothetical study all subjects were observed for a maximum of 10 hours, and some did not reach pain relief, while others got relief afterward varying periods of fourth dimension. We can calculate the average charge per unit of hurting relief in each group by adding upwards the duration of pain for subjects in each group and dividing by the number of subjects in each group.
In the grouping receiving the new drug the times were 4x1 + 2 + 3+ 4x10= 49 hours for the group (person-hours). And so the incidence rate of relief was 6/49 person-hours or on boilerplate 12.2 per 100 person-hours of ascertainment. Note that once a subject experiences the issue of pain relief, they are no longer considered to be under observation.
In the group receiving the old drug the times were 4x7 + viii + 9 + 4x10= 85 hours for the group (person-hours). Then the incidence rate of relief was 6/85 person-hours or on average 7.0 per 100 person-hours of observation. And then, the charge per unit of pain relief was greater in the group receiving the new drug.
What we accept calculated is the incidence charge per unit . This is a true rate, because fourth dimension is an integral function of the calculation, analogous to miles per hour (a charge per unit of speed) or gallons per minute (a rate of flow).
Several things are noteworthy about this incidence rate.
- The numerator is the same for both cumulative incidence and incidence charge per unit; it is the number of individuals who developed the outcome of interest (in this example pain relief) during the observation menstruum.
- The denominators for cumulative incidence and incidence charge per unit are very different. For cumulative incidence, the denominator is the total number of "at risk" subjects being followed; for incidence rate, the denominator is the full corporeality of fourth dimension "at risk" of continued pain for all the subjects who were being followed. Therefore, we tin simply summate an incidence rate if we take periodic follow-up information on each subject area, including not only if they adult the upshot, but also when they developed it.
- The incidence rate is a more accurate estimate of the rate at which the outcome develops. Cumulative incidence is frequently referred to as a 'charge per unit', but it really is the proportion of people who develop the outcome during a fixed block of time. This was useful when we wanted to describe the incidence of AIDS in Massachusetts, considering nosotros didn't have detailed information on each and every resident of the state. We couldn't accept into account when people developed AIDS. Moreover, we couldn't account for people who moved into the state in the heart of the yr or people who moved out or died. With incidence rate, yet, we tin take these factors into account. The strategy is the same as in the hurting relief sample higher up, i.e. the denominator takes into account the full corporeality of "at gamble" time for the group.
- Incidence rates are peculiarly advantageous when trying measure incidence in studies with dynamic populations and in studies with fixed populations with relatively long follow-up time.
Question: A participant in a prospective cohort report or a randomized clinical trial stops contributing additional "illness-complimentary observation fourth dimension" when they develop the outcome of interest or get lost to follow-up for any reason (decease, failure to respond to phone calls, messages and emails, etc.). Does this mean that they are no longer in the report?
Reply
Incidence of HIV in a Brothel
A follow-up study was conducted to decide which sexual behaviors were associated with the greatest gamble of becoming HIV+. The report was conducted in a grouping of female prostitutes. The subjects were tested prior to the first of the study, and 5 HIV+ women were excluded. The the remaining ten women were followed for 6 years beginning in January 1989. Each woman was contacted and retested at the beginning of Jan each twelvemonth. The table below summarizes the findings these x subjects. A circled plus sign (+) indicates when a subject was found to be HIV+; a question mark (?) indicates when a subject field became lost to follow-upward. The dashed lines signal continued follow-up.
Link to a detailed description of the table below
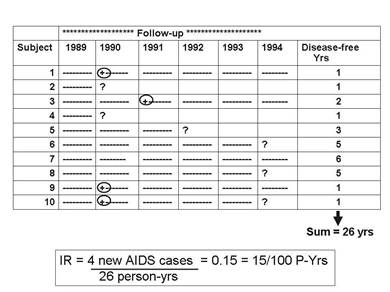
The cumulative incidence was four/10=xl% over vi years, just this doesn't take into account the different amounts of time contributed past those who didn't become HIV positive, ane of whom (Bailiwick #7) was followed throughout the vi years of the study, simply the remainder of whom were lost to follow-upward old before the end of the written report (Subjects #2, 4, 5, six, 8).
The incidence rate , however, tin take these problems into business relationship, considering the denominator is the total "at hazard" observation time contributed past all ten subjects. The column at the far correct indicates each subject'south "at risk" observation fourth dimension, and the sum for the x subjects was 26 years. So, the IR= 4/26 person-yrs = 0.fifteen/person-year = 15/100 person-years of observation.
Annotation that person-time stopped being counted every bit soon as the subject was found to be HIV positive, considering the subject was no longer "at risk" of developing the issue—they already had experienced it. For example, Subject #1 contributed i person-year even though she was followed for all six years.
Incidence rates are ofttimes computed in prospective cohort studies (e.g., The Framingham Heart Report or The Nurses Health Report) and randomized clinical trials (east.g., The Physician's Health Study, which looked at the effect of low-dose aspirin on heart affliction). Information technology is more accurate than cumulative incidence, but it requires repeated follow-up observations on each field of study, and studies like this tin exist very expensive and time consuming.
Also consider that subjects are sometimes recruited into studies at different times. Each subject's disease-free observation time or "at risk" time can be calculated as the fourth dimension from their entry into the report until a) they get the disease, b) they become lost to follow-upwardly, or c) the report ends.
For case, consider a hypothetical clinical trial that was conducted to determine whether taking low-dose aspirin reduced the frequency of heart attacks in middle-aged and elderly men. The time line beneath summarizes events 12 subjects labeled 1-12, all of whom were allocated to the placebo-treated group.
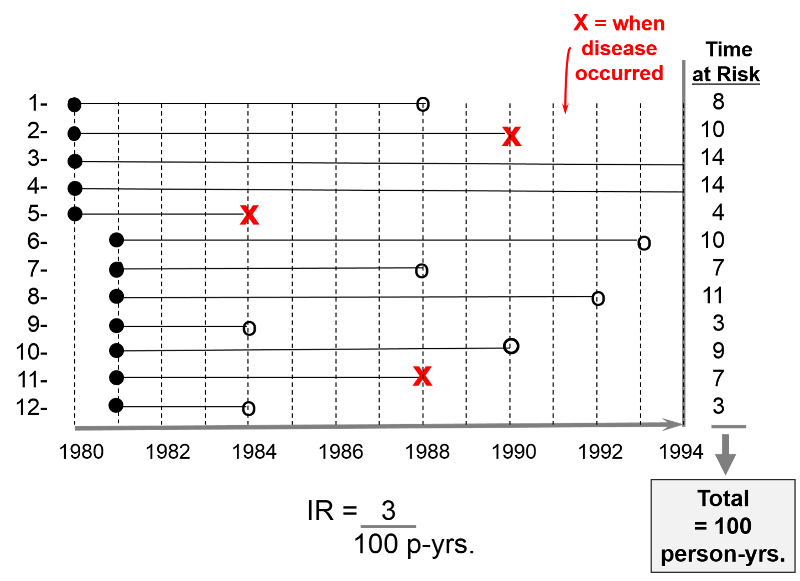
The first 5 subjects were enrolled in 1980, and the next 7 subjects were enrolled 1 yr after. All subjects began taking aspirin upon enrollment. Therefore their "exposure" to aspirin began upon enrollment as indicated by the solid black dots.
The blood-red "Ten"s indicate when subjects had a heart attack; their exposure time at run a risk ends there, since having a first middle attack means that they were no longer at risk of having a get-go heart attack; they had the outcome of interest at that point. Subject #2 had a heart assault in 1990; subject #5 had i in 1984; subject field #11 had one in 1988.
The open circles indicated six subjects who were lost to follow-upwardly. They stopped responding to all requests for follow upward afterwards that point. We know that they had not had a center assault up to that bespeak, only nosotros don't know what happened to them later that, so they finish contributed observed exposure time at risk. Subject #1 was lost to follow up in 1988; #6 was lost in 1993; #7 was lost in 1988; #8 was lost in 1992; #nine was lost in 1984;
All of this information can be taken into business relationship in social club to compute the average rate at which heart attacks occur in this group of 12 men beingness treated with low-dose aspirin. We tin do this in a way that is analogous to example #2 above. In that location were 3 heart attacks, and we divide this by the total corporeality of fourth dimension that the men were exposed and at risk of developing a heart attack. For each man the exposure fourth dimension at adventure is the time from their entry into the study until 1 of 3 endpoints: a) the affliction occurs, b) the subject is lost to follow-upward, or c) the study concludes. The exposure time at risk for each human is shown in the column at the far right of the figure, and if we add these, the total exposure time for the group was 100 years. Therefore, the average rate at which the outcome occurred was three/ 100 person-years of observed exposure time.
Instance: Incidence Rate in the Nurse'due south Health Report - Estrogens and Coronary Avenue Disease
Data nerveless from the Nurses' Health Study, a prospective cohort study, was used to compare rates of coronary artery affliction in post-menopausal women using hormone replacement therapy (HRT) and mail-menopausal women who had not used HRT. The data was summarized in the table beneath.
| Coronary Artery Disease | Person-Years of Affliction Complimentary Observation | |
|---|---|---|
| Used HRT | 30 | 54,308.seven |
| No Utilize of HRT | 60 | 51,477.5 |
Women on postmenopausal hormones had an incidence rate of 30 events during 54,308.seven person years of follow-upward, or 55.2 / 100,000 person-years. Women in the untreated group had 60 events during 51,477.5 person-years of follow-up - an incidence charge per unit of 116.vi / 100,000 person-years.
Another Example: Incidence Rate in the Nurse's Health Study – Obesity and Myocardial Infarction
In this study, incidence rates of MI (myocardial infarction) were compared among v groups of women based on their body mass index (BMI). There were certainly dissimilar numbers of women in the five groups, only for each group they computed the incidence charge per unit by counting the number who adult MI and dividing by the group's total "at run a risk" time of observation. The result was then converted to the number per 100,000 person-years to facilitate comparison amongst the five groups.
| Body Mass Index (BMI) | # Non-fatal Myocardial Infarctions | Person-Years of Ascertainment | Incidence Charge per unit per 100,000 Person-Years |
|---|---|---|---|
| <21 | 41 | 177,356 | 23.1 |
| 21.0-22.nine | 57 | 194,243 | 29.3 |
| 23.0-24.9 | 58 | 155,717 | 36.0 |
| 25.0-29.9 | 67 | 148,541 | 45.ane |
| > 30 | 85 | 99,573 | 85.iv |
Units for Denominators
By convention, all three measures of disease frequency (prevalence, cumulative incidence, and incidence rate) are expressed equally some multiple of 10 in social club to facilitate comparisons. Consider these three examples:
- Cumulative incidence: four/10 over 6 years = 0.xl = 40 per 100 or 40% over 6 years
- Incidence rate: 3/107.7 person-yrs = 0.02785/person-yr = 28 per one,000 person-years
One tin can express the last result as the number of cases per 100 people, or per 1,000 people, or per 10,000 people, or per 100,000. Generally one uses a user-friendly multiple of ten. For instance, the expressions below are all equivalent, merely the last two are the nigh convenient to talk about & recollect about. Note: Each time you move the decimal to the right, y'all increase the number by a factor of 10.
Equivalent Expressions of Illness Frequency
0.00232 new cases per one person-yrs.
0.0232 new cases per x person-yrs.
0.232 new cases per 100 person-yrs.
2.32 new cases per 1,000 person-yrs.
23.2 new cases per ten,000 person-yrs.
232 new cases per 100,000 person-yrs.
 Common Pitfall : A mutual mistake among first students is to neglect to specify the dimensions after computing incidence, especially for cumulative incidence.
Common Pitfall : A mutual mistake among first students is to neglect to specify the dimensions after computing incidence, especially for cumulative incidence.
- In the example for HIV in sexual practice workers, the incidence charge per unit should be reported as fifteen per 100 person-years. Note that this number is non the equivalent of a pct.
- In the same case, the cumulative incidence was 4 per 10 subjects (40%) over half-dozen years. Note: You must specify the fourth dimension period for cumulative incidence or y'all will lose points on the exams.
 Summary of Basic Measures of Disease Frequency
Summary of Basic Measures of Disease Frequency
Prevalence (a proportion)
= People # People with disease at a bespeak in time
Total People # People in the report population
Cumulative Incidence (a proportion)
= People # new cases in a specified period
Full People # People (at risk) in the report population
Incidence Charge per unit (a rate)
= People # new cases of disease
People-Fourth dimension Total ascertainment time in a group at risk

Relationship of Incidence Rate to Cumulative Incidence (Risk)
Cumulative incidence (the proportion of a population at risk that volition develop an outcome in a given period of time) provides a mensurate of gamble, and it is an intuitive way to call up nigh possible wellness outcomes. An incidence rate is less intuitive, because information technology is really an estimate of the instantaneous rate of disease, i.e. the rate at which new cases are occurring at any particular moment. Incidence rate is therefore more analogous to the speed of a car, which is typically expressed in miles per 60 minutes. Time has to elapse to measure a car's speed, but nosotros don't take to wait a whole hour; nosotros tin glance at the speedometer to run into the instantaneous rate of travel. Rather than measuring risk per se, incidence rate measures the charge per unit at which new cases of disease occur per unit of time, and time is an integral part of the calculation of incidence rate. In dissimilarity, cumulative incidence or risk assesses the probability of an result occurring during a stated flow of ascertainment. Consequently, it is essential to depict the relevant fourth dimension period in words when discussing cumulative incidence (risk), but time is not an integral part of the adding. Despite this stardom, these 2 ways of expressing incidence are apparently related, and incidence rate can be used to estimate cumulative incidence. At first glance it would seem logical that, if the incidence rate remained constant the cumulative incidence would exist equal to the incidence rate times fourth dimension:
CI = IR x T
This relationship would concord true if the population were infinitely large, but in a finite population this approximation becomes increasingly inaccurate over time, considering the size of the population at hazard declines over time. Rothman uses the instance of a population of 1,000 people who experience a bloodshed rate of eleven deaths per 1,000 person-years over a menstruum of years; in other words, the charge per unit remains constant. The equation above would lead united states to believe that after l years the cumulative incidence of death would be CI = IR 10 T = 11 Ten l = 550 deaths in a population which initially had 1,000 members. In reality, there would simply be 423 deaths after 50 years. The problem is that the equation above fails to take into account the fact that the size of the population at risk declines over time. After the showtime twelvemonth there have been eleven deaths, and the population now has only 989 people, non 1,000. Every bit a effect, the equation to a higher place overestimates the cumulative incidence, because there is an exponential disuse in the population at risk. A more accurate mathematical expression that takes this into business relationship is:
CI = ane - e(-IR x T), where 'e' = ii.71828
This constant 'e' arises in many mathematical relationships describing growth or decay over time. If you lot are using an Excel spreadsheet, you could calculate the CI using the formula:
CI = 1 - EXP(-IR xT)
In the graph below the upper blue line shows the predicted number of deaths using the approximation CI = IR ten T. The lower line, in red, shows the more accurate projection of cumulative deaths using the exponential equation.
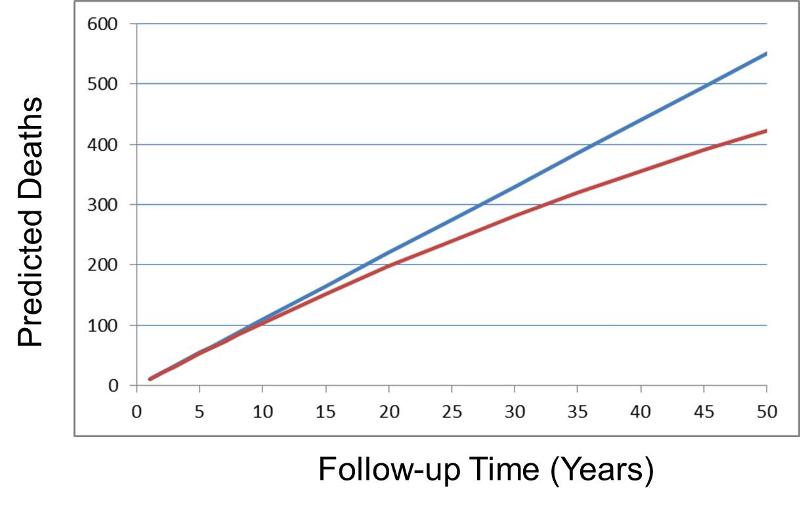
Nevertheless, note that the prediction from CI = IR x T gives quite reasonable estimates equally long every bit the cumulative incidence remains less than 10% (equivalent to 100 deaths in the population of 1,000 in the above graph).
Life Tables and Survival Assay
(Optional)
The equation CI = IR 10 T provides a reasonable gauge of risk when the incidence rate is relatively constant, just this isn't always the instance. When the incidence rate changes over time there are other options for estimating gamble.
- One could calculate risk serially over shorter time intervals during which take chances is reasonably abiding. However, the intervals have to be long enough to enable meaningful incidence rates for each interval.
- Another approach that is useful when risk is changing over time is to use survival assay . Despite the name, it tin exist used for whatsoever outcome regardless of whether it is fatal or not. The tabular array below shows a hypothetical life-table cited by Rothman.
Table - Life-table for Death from Motor-vehicle Injury from Bitth through Age 85
| Age (years) | Bloodshed Charge per unit per 100,000 person-years | At Risk | Deaths in Interval | Adventure | Survival Probability | Cumulative Survival Probability |
|---|---|---|---|---|---|---|
| 0-fourteen | 4.7 | 100,000 | lxx.five | 0.000705 | 0.999295 | 0.999295 |
| xv-24 | 35.9 | 99,930 | 358.ane | 0.003584 | 0.996416 | 0.995714 |
| 25-44 | 20.1 | 99,571 | 399.5 | 0.004012 | 0.995988 | 0.991719 |
| 45-64 | 18.four | 99,172 | 364.three | 0.003673 | 0.996327 | 0.988077 |
| 65-84 | 21.7 | 98,808 | 427.9 | 0.004331 | 0.995669 | 0.983798 |
Adjusted from Iskrant and Joliet
In this hypothetical example, the initial population at gamble was arbitrarily set up at 100,000, and the bloodshed rates in each group (column two, bloodshed rates=deaths per 100,000 person-yrs.) were used to calculate the number of deaths amongst those remaining at gamble for each interval using the formula CI = IR x T. Thus, the start age group spanned 15 years and the mortality charge per unit was 4.vii/100,000 person-years, so the number of deaths was four.vii x xv = 70.5.
The illustration beneath shows the results of assay of a trial looking at the ability of zidovudine (an anti-retroviral drug used in the treatment and prevention of HIV) to reduce maternal to kid transmission. Pegnant women with mildly symptomatic HIV disease and no prior treatment with antiretroviral drugs during the pregnancy, were randomly assigned to i of two regimens: 1) a regimen consisting of zidovudine given ante partum and intra partum to the female parent and to the newborn for vi weeks or 2) placebo.
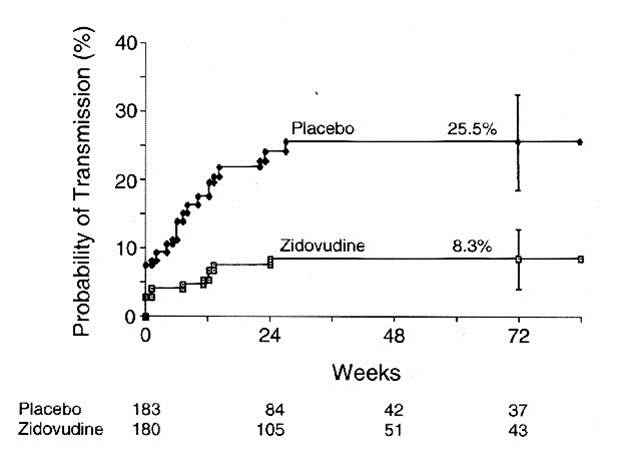
The graph shows that well-nigh 8 % of the infants in the placebo grouping tested HIV+ at birth, and the probability of HIV transmission in this group rose to 25.v% past 72 weeks of historic period. Infants in the zidovudine group only had about a 3% probablility of being built-in HIV+, and their take chances of transmission just todr yo viii.iii% by 72 weeks of age. (The data are from Connor EM, et al.: Reduction in maternal-infant manual of human immunodeficiency virus blazon 1 with zidovudine treatment. N. Engl. J. Med. 1994;331:1173-1180, every bit quoted in the textbook by Aschengrau and Seage in Table 7-v, folio 191 in the 2nd edition.) This was role of protocol 076 that originally demonstrated the efficacy of zidovudine in women in the United States and France. The analogy below shows Kaplan-Meier plots of the probability of HIV transmission for the two groups. The estimated percentages of infants infected at 72 weeks are shown with 95 percent confidence intervals. The numbers of infants at adventure at 24, 48, and 72 weeks are shown below the figure.

Relationship Amid Prevalence, Incidence Rate, and Boilerplate Duration of Disease
Prevalence is the proportion of a population that has a condition at a specific time, but the prevalence will be influenced by both the rate at which new cases are occurring and the average duration of the affliction. Incidence reflects the rate at which new cases of disease are beingness added to the population (and becoming prevalent cases). Average elapsing of affliction is likewise of import, because the only style you tin end being a prevalent instance is to be cured or to motion out of the population or die. For example, about a decade agone the average elapsing of lung cancer was near six months. Therapy was ineffective and most all lung cancer cases died. From the time of diagnosis, the average survival was only about six months. And so, the prevalence of lung cancer was fairly depression. In contrast, diabetes has a long average duration, since it can't be cured, but it can be controlled with medications, so the boilerplate duration of diabetes is long, and the prevalence is fairly loftier.
If the population is initially in a "steady state," pregnant that prevalence is fairly constant and incidence and outflow [cure and death] are about equal), and so the human relationship amid these three parameters tin can be described mathematically as:
P/(one-P) = IR x Avg. Duration ,
where P= proportion of the population with the disease and (one-P) is the proportion without it, IR is the incidence rate, and Avg. Elapsing is the boilerplate fourth dimension that people have the disease (from diagnosis until they are either cured or die). If the frequency of disease is rare (i.e., <10% of the population has it), then the relationship tin be expressed equally follow:
Prevalence = (Incidence Rate) 10 (Average Duration of Disease)
- If the boilerplate duration of illness remains constant, and so preventive measures that reduce the incidence of disease would be expected to result in a decreased prevalence.
- Similarly, if the incidence remained constant, then developing a cure would reduce the average elapsing of affliction, and this would as well reduce the prevalence of disease.
- In the tardily 1990s anti-retroviral therapy was introduced and profoundly improved the survival of people with HIV. However, they weren't cured of their disease, meaning that the average duration of disease increased. Every bit a result, the prevalence of HIV increased during this period.
The relationship can be visualized past thinking of arrival and outflow from a reservoir. The fullness of the reservoir can be idea of every bit coordinating to prevalence. Raindrops might represent incidence or the rate at which new cases of a disease are being added to the population, thus condign prevalent cases. Water also flows out of the reservoir, analogous to removal of prevalent cases by virtue of either dying or being cured of the illness. Imagine that incidence (rainfall) and the rate of cure or expiry are initially equal; if so, the height of water in the reservoir volition remain abiding.
- If outflow from the reservoir (rates of cure or decease among prevalent cases) remains constant and rainfall (incidence of new illness) increases, then the top of water in the reservoir will rise. Conversely, if incidence (rainfall) declines, and then the water level volition fall.
- If we start from steady state again, and the rate of rainfall remains constant, but the outflow (rate of cure or rate of death) increases, so the pinnacle of the h2o (prevalence) will fall. Conversely, if incidence is held constant, but outflow falls (eastward.grand., if the lives of prevalent cases are prolonged, simply they aren't cured, and so the top of the water will rise.
Calculating Average Duration of Disease
This relationship tin also be used to calculate the average duration of affliction under steady state circumstances. If Prevalence = (Incidence) Ten (Average Elapsing), then it follows that
Average Duration = (Prevalence) / (Incidence)
Example: Suppose the incidence charge per unit of lung cancer is 46 new cancers per 100,000 P-Y, and the prevalence is 23 per 100,000 population, and so
Average Duration of Disease = (23/100,000 persons / 46/100,000 person-years = 0.5 year
Decision: Individuals with lung cancer survived an boilerplate of 6 months from the time of diagnosis to expiry.



Special Types of Frequency Measures
Prevalence and incidence are the primal measures of disease frequency, but special names have evolved for these measures, depending on their specific use. All of these tend to be referred to as rates, even though, strictly speaking, they oft refer to proportions (cumulative incidence or prevalence).
Category-specific Rates
Either prevalence or incidence can exist broken down into categoies, e.k., age groups, or by gender, or race, or some combination of these. For instance, since disease frequency oft differs substantially with age, one frequently sees "age-specific" rates of disease.
Example 1: A tabular array of age-specific rates of stroke (incidence)
| Age Group | # New Occurrences | Group Size | Cumulative Incidence per 100,000 persons |
|---|---|---|---|
| 0-34 | 0 | 582,083 | 0 |
| 35-44 | 28 | 113,581 | 25 |
| 45-54 | 114 | 114,208 | 100 |
| 55-64 | 320 | 91,484 | 350 |
| 65-74 | 550 | 81,155 | 900 |
| 75+ | 1.126 | 37,531 | 3,000 |
Instance 2: A Table of race-specific causes of death per 100,000 population (bloodshed rates, i.e., incidence) in the US, 1967
| White | Blackness | |
|---|---|---|
| Hypertension | 21.1 | 68.6 |
| Homicide | iii.5 | 32.3 |
| Diabetes mellitus | 16.6 | 28.9 |
| Tuberculosis | 2.5 | 9.6 |
| Suicide | xi.three | 5.7 |
| Leukemia | 7.4 | five.5 |
| Syphilis | 1.0 | 3.0 |
Interesting Visual Bout of Causes of Death in the United states
Special Measures of Incidence
Morbidity rate is the incidence of not-fatal cases of a illness in a population during a specified time flow. For example, during 1982 in that location were 25,520 not-fatal cases of TB in the The states population. The mid-year population was estimated at 231,534,000. Therefore, the
Morbidity rate of TB =25,520/231,534,000 = eleven.0/100,000 over one year
Note that this is a cumulative incidence and therefore is really a proportion, not a true rate.)
Bloodshed Rate: In 1982 at that place were 1,807 deaths from TB in the Usa population, then the bloodshed rate for TB was 7.8 per 1000000 over one year (also a cumulative incidence, not a true charge per unit).
Case-Fatality Rate: the number of deaths from a specific illness divided by the full number of cases of that affliction, i.e. the proportion of fatal cases of a disease (%). This provides a measure of the severity of the disease.
Example: Reyes Syndrome is a rare, only highly fatal disease in which the liver and brain become dysfunctional due to abnormal aggregating of cellular fat. It tends to occur when people are recovering from a viral illness, and it tends to exist associated with utilise of aspirin, especially in children. If there were 200 cases of Reyes syndrome in 1982 and 70 died, then the example-fatality rate would be 70/200 = 35% over one year.
[Notation: This is generally calculated by dividing the deaths reported in a given year by the number of cases reported in the same year, but this can exist misleading since some diseases (e.g., TB) aren't apace fatal. Thus, many of the TB fatalities that occurred in 1982 were due to cases diagnosed several years before.]
Attack Rate: a cumulative incidence for a disease during a specific period (e.yard., an epidemic).
Example: After a church picnic in Oswego, NY many attendees got food poisoning. At that place were 75 people at the picnic; 46 got sick inside several hours, so the assault charge per unit was 46/75 = 61%.
Live birth rate: the frequency of live births in one year per 1,000 females of childbearing age.
Infant Bloodshed Rate: the frequency of deaths in children nether 1 year of age occurring during a 1 twelvemonth catamenia per 1,000 live births.
Special Prevalence Measures
These are ofttimes incorrectly referred to as incidences or rates, merely they are, in fact, proportions..
Dissection Rate : the proportion of people who accept a particular finding on a postmortem exam (the prevalence of a certain finding among the population of people who get autopsied).
Birth Defect Charge per unit : the prevalence of a built aberration at the "signal" of nascency. The denominator can be either live births or total births (which includes live births + stillbirths), merely it by and large does not include spontaneously aborted fetuses.
The Obstruction Grade

Questions to test your agreement

A sample of 100 heart aged and elderly women was followed prospectively for 10 years in order to study rates of ovarian cancer. All subjects entered the study on January 1, 1990, and all were free of cancer at the offset. All women were followed until December 31, 1999. None were lost to follow-up. During this period, 5 subjects were diagnosed with ovarian cancer, but they all survived to the end of the study.
Case #1 was diagnosed with ovarian cancer in January 1991.
Instance #ii was diagnosed in January 1992.
Case #3 was diagnosed in January 1993.
Example #four was diagnosed in January 1986.
Instance #5 was diagnosed in January 1996.
The time at which these five subjects developed cancer is shown in this table:
Employ this information and the data in the table below to respond the questions below the tabl:
| Discipline | 1990 | 1991 | 1992 | 1993 | 1994 | 1995 | 1996 | 1997 | 1998 | 1999 |
|---|---|---|---|---|---|---|---|---|---|---|
| Case #1 | cancer | |||||||||
| Case #2 | cancer | |||||||||
| Instance #three | cancer | |||||||||
| Example #4 | cancer | |||||||||
| Case #5 | cancer |





Use this data and the information in the table beneath to respond the questions below the table:
In January of 1990, 1,010 young adults offered to participate in a x-year prospective report to determine their risk of Type-I diabetes. This group underwent an initial blood exam to determine whether they were diabetic, and eligible subjects were re-tested yearly for the next x years. Amid the group that offered to join the report:
- There were 2 individuals who were found to have diabetes on the initial blood screening; these 2 people were referred for treatment and were not enrolled in the written report
- There were 1,000 who were affliction-free and remained disease-free for the entire x years of the study
- 6 individuals developed diabetes during the course of the report at the times indicated in the tabular array beneath
- ii individuals who were initially disease-free were lost to follow-up during the study at the times indicated in the table beneath
? = Lost to follow-up + = Blood test positive for diabetes ------ = Continued disease-free follow-upwards
| Subject # | 1990 | 1991 | 1992 | 1993 | 1994 | 1995 | 1996 | 1997 | 1998 | 1999 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | ------ | ------ | + | |||||||
| ii | ------ | ------ | ------ | ------ | ------ | ------ | ------ | ------ | ------ | + |
| 3 | ------ | ------ | ------ | ------ | ------ | ------ | ------ | + | ||
| 4 | ------ | + | ||||||||
| 5 | ------ | ------ | ------ | ------ | + | |||||
| 6 | ------ | ------ | + | |||||||
| 7 | ------ | ------ | ------ | ------ | ? | |||||
| 8 | ------ | ------ | ------ | ------ | ------ | ? |






Source: https://sphweb.bumc.bu.edu/otlt/mph-modules/ep/ep713_diseasefrequency/ep713_diseasefrequency_print.html
Posted by: liddellpacconte.blogspot.com


0 Response to "Which Of The Following Can Change The Frequency Of Resistant Cells In A Population Of Bacteria?"
Post a Comment